PREDICTIVE FACTORS OF SUCCESSFUL RETURN OF SPONTANEOUS CIRCULATION (ROSC) IN OUT-OF-HOSPITAL CARDIAC ARREST – A NATIONAL STUDY
Introduction
Out-of-Hospital Cardiac Arrest (OHCA) represents one of the primary challenges in global healthcare and is a significant cause of mortality worldwide. Despite substantial advancements in cardiopulmonary resuscitation (CPR) techniques and the widespread implementation of early defibrillation strategies, the survival rate of patients experiencing OHCA remains unsatisfactory (1). The global incidence of this condition is high, posing a serious health threat that necessitates continuous efforts to improve access to emergency medical services and public education.
Survival following OHCA varies significantly depending on geographic location, emergency medical service infrastructure, and the level of bystander education.
Even in highly developed countries with well-equipped healthcare systems and extensive emergency service coverage, survival rates often remain below 10 % (2).
These statistics not only highlight variability in clinical outcomes but also underscore the complexity of factors influencing resuscitation success. Key determinants include the availability and response time of emergency services, as well as the ability and willingness of bystanders to promptly and effectively perform CPR.
The outcomes of OHCA are also closely linked to sociodemographic and clinical characteristics of patients, including age, sex, pre-existing medical conditions, and specific circumstances such as the location and timing of cardiac arrest. Elderly patients or those with pre-existing cardiovascular diseases often have poorer prognoses (3). Additionally, socioeconomic factors, such as access to medical care and individual educational status, can significantly influence the likelihood and outcome of an intervention.
Out-of-hospital cardiac arrest has low survival rates worldwide, with early bystander action, fast emergency response, and initial rhythm crucial; return of spontaneous circulation predicts outcomes.
Return of Spontaneous Circulation (ROSC) is a key objective of emergency medical intervention following OHCA and is considered an essential indicator of resuscitation quality.
Achieving ROSC is not only a critical step in stabilizing the patient but also a significant predictor of long-term survival and post-arrest quality of life (1). In the context of acute medical care, rapid and effective resuscitation leading to ROSC can substantially reduce in-hospital mortality and improve recovery outcomes.
Several key factors influence resuscitation outcomes and the likelihood of successful ROSC, including the initial cardiac arrest rhythm, patient age and sex, and the presence of bystanders capable of providing early resuscitation measures (4). Initial cardiac arrest rhythms such as ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT) are associated with a higher likelihood of successful ROSC due to their greater responsiveness to defibrillation. Conversely, asystole and pulseless electrical activity (PEA) often indicate poorer prognoses and require more complex and prolonged interventions to achieve ROSC (5).
The presence of bystanders plays a crucial role in OHCA outcomes, as they can initiate CPR and potentially use an Automated External Defibrillator (AED), significantly increasing survival chances (6). The application of an AED by bystanders before emergency services arrive is particularly critical in cases of VF and VT, where each minute without defibrillation decreases survival probability by 7 % to 10 % (7).
In Croatia, the organization of emergency medical services is structured at the county level through Emergency Medicine Institutes. The emergency medicine network regulates the number, composition, and types of teams operating in different regions to ensure nationwide coverage. This system ensures that at least one emergency team is available within a 25-kilometer radius. Overall, there are 709 Type 1 (T1) teams, 205 Type 2 (T2) teams, and 31 standby teams across 21 county emergency institutes. A T1 team consists of a medical doctor, a nurse, and a driver, while a T2 team includes a specialized nurse or technician and a driver. Emergency services are organized through ambulance transport, with helicopter services available for secondary interventions on islands (8).
Emergency medical services in Croatia are organized by county, ensuring full coverage with T1 and T2 teams available within 25 km, including helicopter support for islands.
The aim of this study was to analyze predictive factors for successful return of spontaneous circulation in out-of-hospital cardiac arrests, considering the initiation of bystander CPR before the arrival of emergency medical teams, the initial cardiac arrest rhythm, and regional differences.
Methods and patients
This prospective study included adult patients who experienced sudden cardiac arrest in out-of-hospital settings. Data were collected from January 1, 2024, to December 31, 2024. The study encompassed all adult patients who suffered sudden cardiac arrest in out-of-hospital conditions within the territory of the Republic of Croatia.
For data collection, the standardized Utstein template was used, which is a mandatory part of medical documentation in out-of-hospital emergency medical services (according to Article 19, Annex 7 of the Regulation on Conditions, Organization, and Mode of Emergency Medicine
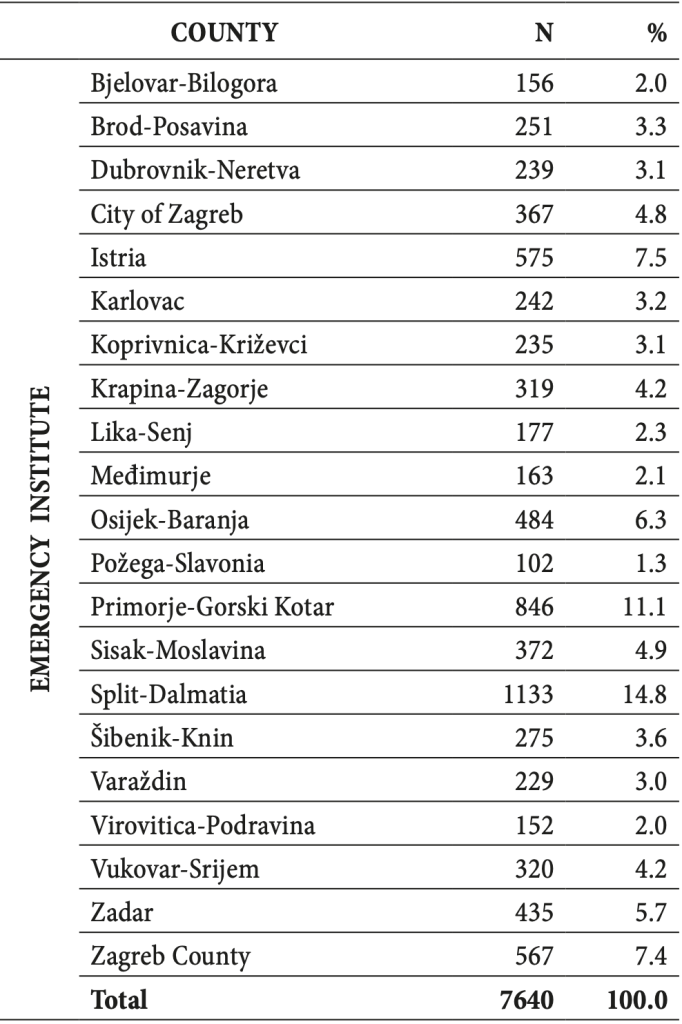
Table 1. Distribution of Participants by County
Operations, Official Gazette 71/2016). The form was completed by emergency medical service personnel who had been previously trained in proper documentation procedures. Additionally, Emergency Medicine Institutes received written instructions to standardize data collection according to the recommendations of the International Liaison Committee on Resuscitation (ILCOR).
The collected data included general patient characteristics such as age, cause, and location of the event. Event and outcome-related data encompassed the provision of telephone CPR instructions, bystander CPR, initial cardiac arrest rhythm, and the presence of signs of life upon hospital admission.
Statistical Methods
Data were analyzed using the IBM SPSS Statistics software (version 25.0). Continuous variables (age) were assessed for normal distribution using the Kolmogorov-Smirnov test.
The data were presented as means and standard deviations.
Categorical variables were reported as absolute and relative frequencies. Differences between groups were analyzed using the χ² test for categorical variables.
Binary logistic regression was employed to model predictive variables associated with successful ROSC before hospital arrival. Statistical significance was set at p < 0.05
Results
Participants based on regional distribution The local distribution of participants included in the study (N = 7.640) is presented in Table 1. The highest number of participants was recorded in Split-Dalmatia County, with 1.133 (14.8 %), while the lowest number was observed in Požega-Slavonia County, with 102 (1.3 %).
Sociodemographic and clinical characteristics of participants
The study included 7.640 participants, with asystole being the predominant cardiac arrest rhythm (46.5 %). Medical causes accounted for the majority of cardiac arrests (72.0 %). Signs of life during CPR were recorded in 10 % of participants, while at the time of hospitalization, this percentage dropped to 7.5 %, indicating a low survival rate to hospital admission. Most participants were male (64.9 %) with an average age of 70.77 years, which aligns with epidemiological data suggesting a higher prevalence of cardiovascular diseases among older men (Table 2).
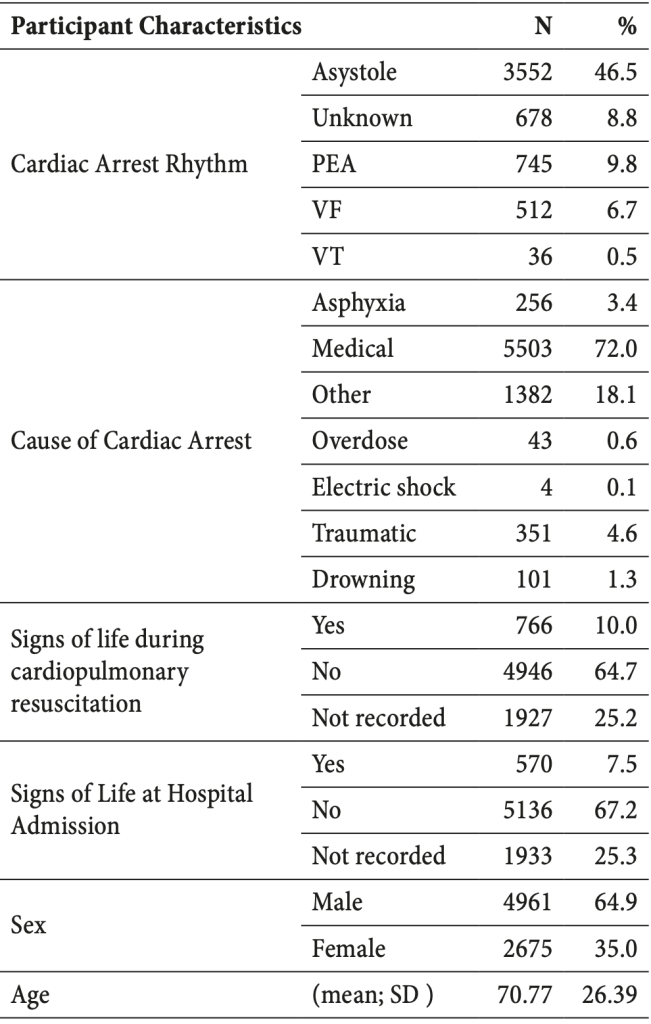
Table 2. Sociodemographic and Clinical Characteristics
of Participants
Resuscitation depending on initiation of bystander CPR before Emergency Mecial Services (EMS) team arrival
Data on both the outcome and the initiation of bystander CPR were recorded for 4.315 participants. The results indicate a statistically significant association between initiated bystander resuscitation and the ROSC outcome (p < 0,001) (Table 3). Among participants who received bystander CPR, 33.2 % achieved successful ROSC, while 19.5 % did not. In contrast, among those who did not receive bystander CPR, 44.4 % achieved ROSC, whereas 55.9 % had a negaative outcome. Although the success rate of ROSC appears higher in the non-bystander CPR group, the significantly higher proportion of unsuccessful resuscitations in this group suggests that bystander CPR may play a critical role in reducing the total number of unsuccessful resuscitations. These findings highlight the importance of public education on basic life support (BLS) techniques to improve survival rates before emergency medical services (EMS) arrive.
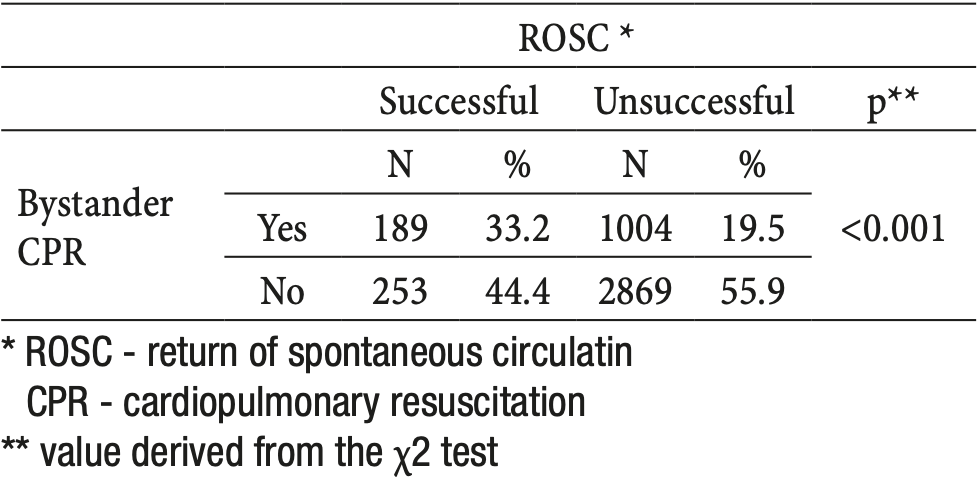
Table 3. Outcome of Resuscitation Based on Initiated Bystander CPR
Outcome of the resuscitation procedure depending on initial rhythm
Data on the outcome of the resuscitation procedure based on the initial rhythm was available for 5706 participants.
The results show a statistically significant association between the initial rhythm of cardiac arrest and the outcome of ROSC (p < 0.001). The highest ROSC success rate was seen with ventricular fibrillation (VF) at 34.6 %.
Patients with asystole, the most common initial rhythm, had a successful ROSC in only 18.6% of cases, while 53.1% of cases resulted in an unsuccessful resuscitation. Pulseless Electrical Activity (PEA) recorded 21.1 % successful and 9.9 % unsuccessful ROSC (Table 4). The results confirm that the initial rhythm significantly influences the outcome of resuscitation, with VF having the best prognosis, while asystole and VT indicate lower chances for the return of spontaneous circulation.
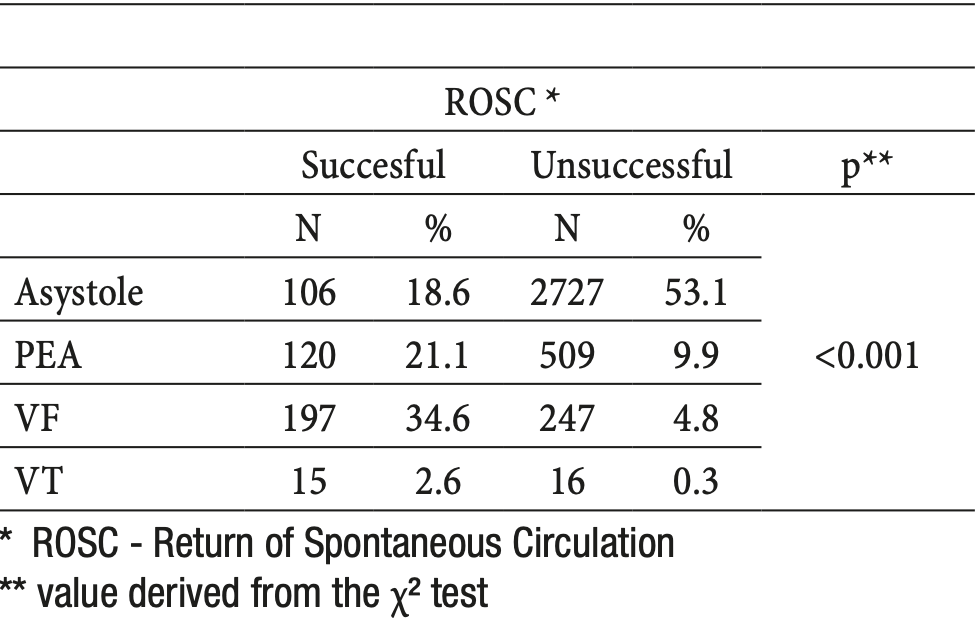
Table 4. Outcome of the Resuscitation Procedure Depending on Initial Rhythm
Regional differences in ROSC outcomes
The results show a statistically significant difference in the outcome of ROSC among counties (p < 0.001) (Table 5), with the City of Zagreb recording the highest proportion of successful ROSCs (14.9 %), while the Split-Dalmatia County had the highest proportion of unsuccessful cases (15.1 %).
Counties with higher percentages of successful ROSC include Istria (10.0 %) and Zagreb (6.0%), while lower percentages of successful cases were recorded in counties such as Virovitica-Podravina (2.3 %) and Međimurje (1.9 %).
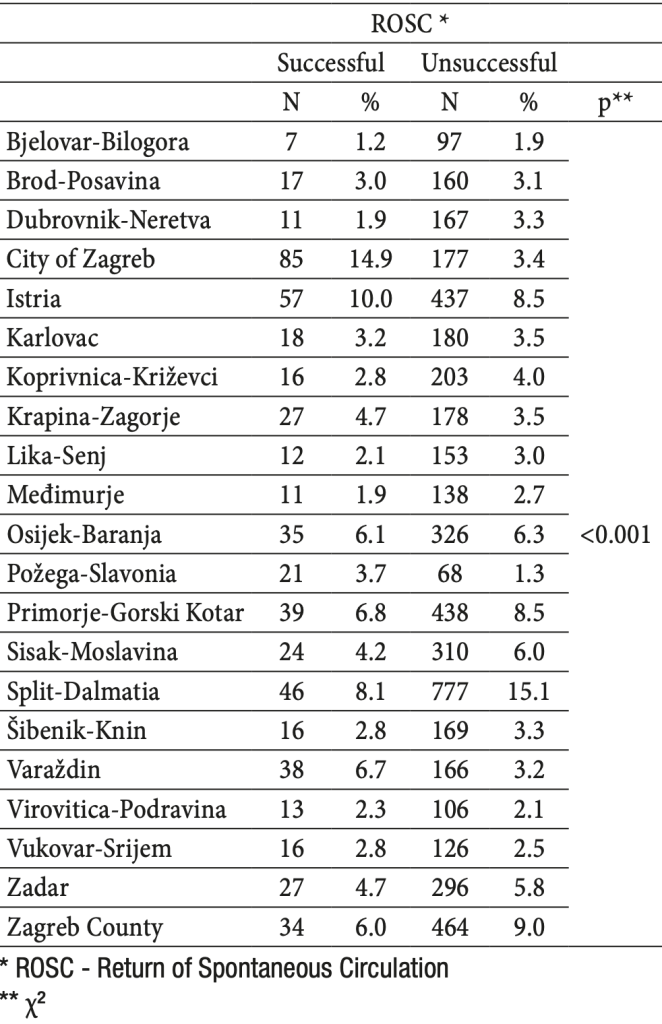
Table 5. Differences in ROSC Outcomes by County
Logistic regression analysis for predicting ROSC
Table 6 presents the results of logistic regression for predicting the likelihood of achieving return of spontaneous circulation (ROSC) by the time of hospital arrival. Among the predictors, age is negatively associated with the outcome, with the probability of ROSC decreasing as age increases [odds ratio (OR) = 0.989, p = 0.003].
Providing layperson CPR has a negative, but weak effect (OR = 0.768, p = 0.034), while providing professional CPR has a highly positive and significant effect (OR = 57 268, p < 0.001). The model explains 26,9 % of the variability in the outcome, highlighting the significance of the included predictors for predicting the outcome.
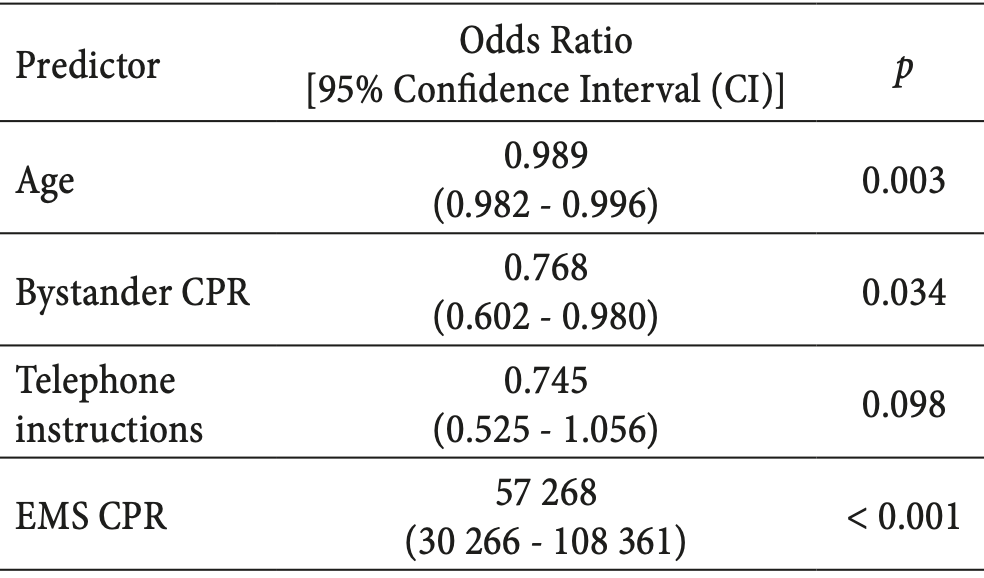
Table 6. Logistic Regression Results for ROSC
Discussion
The results of this study provide a detailed insight into the factors that significantly affect the success of return of spontaneous circulation after out-of-hospital cardiac arrest in the Republic of Croatia. The analysis shown in Table 3 highlights the significant role of layperson CPR before the arrival of professional medical services, with a ROSC success rate of 33,2 % compared to 19,5 % in cases where layperson CPR was not successfully performed. This data confirms the critical importance of early CPR intervention by bystanders, consistent with the findings of Bednarz et al., who concluded that timely CPR intervention generally improves outcomes for patients after OHCA (9). These findings align with the study by Tabata et al. in Japan, which found that layperson CPR training was associated with higher ROSC rates in patients with out-of-hospital cardiac arrest, pointing to the potential benefits of CPR training for non-healthcare professionals (10). Furthermore, research by Siman-Tov et al. in Israel also supports the notion that victims of out-of-hospital cardiac arrest who receive CPR with dispatcher assistance have higher ROSC rates and more frequent defibrillatory rhythms, indicating the universal value of early intervention in improving OHCA outcomes (11).
International studies also emphasize the importance of public education on CPR techniques and the use of automated external defibrillators (AEDs). A study conducted by Leeb in New York (12) demonstrated that training civilians can significantly increase intervention success, similar to trends observed in our study. These data suggest that educational programs and policies promoting widespread CPR application are crucial for improving outcomes in OHCA patients, regardless of geographical location.
A more detailed analysis of the impact of the initial rhythm of cardiac arrest on ROSC outcomes, presented in Table 4, reveals that ventricular fibrillation (VF) has the highest ROSC success rate at 34.6 %. These results are consistent with the research by Kajino et al. (13), who highlighted that VF, due to its high sensitivity to defibrillation, offers better prognosis compared to other rhythms such as asystole or PEA, which require more complex and prolonged resuscitation procedures. Comparing our results to other relevant studies, such as the one by Wolbinski et al. (14), who also emphasized the advantage of VF over asystole and PEA in the context of out-of-hospital cardiac arrest, further supports global consistency in clinical outcomes related to initial rhythms. Additionally, the study by Meneya et al. (15) for the American Heart Association confirms similar trends, showing that patients with VF have a higher survival rate on hospital arrival compared to those with asystole, further supporting the need for prompt and efficient defibrillation as a key element in resuscitation efforts. According to a study by Bergman et al. (16), VF was identified as the most important predictive factor for successful ROSC and long-term survival following cardiac arrest, which matches our results and highlights the importance of continuous monitoring and education in AED use in public spaces.
Regional variations in ROSC outcomes, documented in Table 5, show significant differences within the country, with particularly high success rates recorded in the City of Zagreb (14.9 %). This result may reflect differences in the availability of resources, expertise, and emergency medical service equipment, suggesting the need to strengthen the healthcare system, especially in counties with lower success rates. Potential solutions include improving education for emergency medical personnel, increasing the availability and quality of medical equipment, and enhancing public awareness and education on CPR and AED use.
Regional variations in ROSC outcomes in Croatia show higher success in urban areas like Zagreb, highlighting the need for better resources and training in less equipped regions.
These regional variations are not unique to Croatia. Similar results have been observed in studies from other countries.
For example, a study from the United States showed that urban areas have better outcomes in OHCA cases compared to rural areas, attributed to better access and quicker emergency service interventions (17). In Scandinavia, research conducted in Sweden highlighted that integrated emergency services in larger cities like Stockholm achieve higher successful ROSC rates due to efficient protocols and widespread use of AEDs (18). A study from South Korea highlighted that ongoing public education efforts regarding CPR significantly increase the chances of a successful ROSC, particularly in areas where there previously was low awareness of the importance of early intervention (19).
Logistic regression, shown in Table 6, identifies older age as a factor negatively correlated with ROSC outcomes, implying that each additional year of age reduces the chances of successful ROSC (OR = 0.989; p = 0.003). This aligns with widely accepted scientific knowledge confirming that older patients, due to the presence of comorbidities and reduced physiological capacity, often have poorer outcomes after OHCA (20). This correlation between older age and reduced chances for ROSC has also been documented in several international studies. For instance, research conducted in Poland by Lewandowski et al. also demonstrated that as age increases, the likelihood of return of spontaneous circulation decreases, with a particularly significant drop among individuals over 75 years of age (21). Similarly, some studies highlight that there may be resistance to providing maximally aggressive treatment to all patients due to concerns about creating a larger number of survivors with poor functional outcomes (3, 22). These attitudes underline the need to develop specific strategies for managing cardiac arrest in older patients, including rapid diagnosis and tailored resuscitation that takess their special needs and limitations into account.
These international findings suggest that healthcare systems should consider adjusting their resuscitation protocols to improve outcomes for the older population, particularly by strengthening the capacity and education of healthcare providers for interventions tailored to age-specific risk factors and comorbidities. In an international context, the effectiveness of layperson CPR in Croatia is comparable to that observed in other European countries, where it is also recognized as a key factor in improving OHCA outcomes (23). For example, the document “Education, Implementation, and Teams: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations” suggests that implementing widely accessible layperson CPR education can significantly improve ROSC rates, confirming the importance of early intervention (24). Similar guidelines have been proposed by Ravindra et al., who note that strategies such as social media campaigns can improve awareness, knowledge, and skills related to CPR (25). However, the regional differences present within the country point to the necessity of adapting and implementing locally oriented interventions that consider the specific conditions, resources, and needs of individual regions. In this context, research from North America (26) has shown that regional protocols and specialized education can significantly improve responses to OHCA, especially in rural areas where response times are longer. These results point to the need for regionally tailored programs that could include mobile teams and trained volunteers to support standard emergency services. In analyzing the Swedish model, Strömsöe et al. conducted a study to describe the application of a CPR education program in Sweden over 25 years and link the data to changes in the percentage of OHCA patients who received CPR from bystanders. In Sweden, CPR education is conducted on a cascade principle: instructor-trainers train educators, who then train rescuers.
Widespread layperson CPR education via regional programs like Sweden’s cascade training and North America’s local protocols can improve OHCA outcomes, especially in underserved areas, by increasing early intervention and reducing ROSC disparities.
Since 1989, 5.000 instructor-trainers have trained more than 50.000 educators, who have in turn trained nearly 2 million of Sweden’s 9 million inhabitants in adult CPR. As a result, the number of layperson CPR attempts in OHCA in Sweden increased from 31 % in 1992 to 55 % in 2007, which could be applicable in the context of Croatia given the similar model of education. Such models, based on broad social cooperation and support, could be key to addressing regional disparities in OHCA outcomes.
Limitations of the study
Despite the use of a national data registry, there are limitations related to the potential variability in documentation and reporting of cases from different parts of the country, which may result in incomplete data on some OHCA cases. Furthermore, the availability of variables within the registry does not encompass all clinically relevant factors that could affect outcomes, potentially limiting the comprehensiveness of the analysis.
Also, the study primarily relies on short-term outcomes after resuscitation, without considering long-term survival results and the quality of life of patients, which are key elements for a comprehensive evaluation of CPR intervention effectiveness.
Conclusion
The results of this study clearly demonstrate that early layperson intervention, the initial rhythm of cardiac arrest, and regional disparities are key factors influencing the outcome of return of spontaneous circulation following out-of-hospital cardiac arrests in Croatia. Timely initiation of layperson CPR before the arrival of emergency services significantly increases the chances of a successful ROSC, underscoring the critical importance of expanding CPR training among civilians. Furthermore, ventricular fibrillation as the initial rhythm notably improves the chances of successful resuscitation, highlighting the need for prompt defibrillation. Additionally, regional variations in infrastructure and access to emergency medical care reflect the variability in resuscitation outcomes, suggesting the need for the enhancement and adaptation of healthcare resources and strategies.
References
- Reynolds JC, Frisch A, Rittenberger JC, Callaway CW. Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: when should we change to novel therapies? Circulation. 2013;128(23):2488-94. doi: 10.1161/CIRCULATIONAHA.113.003366.
- Hayashi M, Iwasaki YK. Addressing out-of-hospital cardiac arrest with current technology advances: Breaking the deadlock with a mobile network. J Arrhythm. 2024;40(4):753-66. doi: 10.1002/joa3.12843.
- Hiemstra B, Bergman R, Absalom AR, van der Naalt J, van der Harst P, de Vos R, et al. Long-term outcome of elderly out-of-hospital cardiac arrest survivors as compared with their younger counterparts and the general population. Ther Adv Cardiovasc Dis. 2018;12(12):341-9. doi:10.1177/1753944718800763.
- Cheng P, Yang P, Zhang H, Wang H. Prediction Models for Return of Spontaneous Circulation in Patients with Cardiac Arrest: A Systematic Review and Critical Appraisal. Emerg Med Int. 2023;2023:6780941. doi:10.1155/2023/6780941.
- Morris MC, Todres ID, Schleien CL. Cardiopulmonary Resuscitation. In: Coté CJ, Lerman J, Todres ID, editors. A Practice of Anesthesia for Infants and Children. 4th ed. W.B. Saunders; 2009. p. 833-45. Available from: https://www.sciencedirect.com/science/article/pii/B9781416031345500445.
- Oliveira NC, Oliveira H, Silva TLC, Boné M, Bonito J. The role of bystander CPR in out-of-hospital cardiac arrest: what the evidence tells us. Hellenic J Cardiol. 2024. doi: 10.1016/j.hjc.2024.01.001.
- Ibrahim WH. Recent advances and controversies in adult cardiopulmonary resuscitation. Postgrad Med J. 2007;83(984):649-54. doi: 10.1136/pgmj.2006.054039.
- Važanić D, Prkačin I, Nesek-Adam V, Kurtović B, Rotim C. Out-Of-Hospital Cardiac Arrest Outcomes – Bystander Cardiopulmonary Resuscitation Rate Improvement. Acta Clin Croat. 2022;61(2):265-72. doi: 10.20471/acc.2022.61.02.13
- Bednarz K, Goniewicz K, Al-Wathinani AM, Goniewicz M. Emergency Medicine Perspectives: The Importance of Bystanders and Their Impact on On-Site Resuscitation Measures and Immediate Outcomes of Out-of-Hospital Cardiac Arrest. J Clin Med. 2023;12(21):6815. doi: 10.3390/jcm12216815.
- Tabata R, Tagami T, Suzuki K, Amano T, Takahashi H, Numata H, et al. Effect of cardiopulmonary resuscitation training for layperson bystanders on outcomes of out-of-hospital cardiac arrest: A prospective multicenter observational study. Resuscitation. 2024;201:110314. doi: 10.1016/j.resuscitation.2024.110314.
- Siman-Tov M, Strugo R, Podolsky T, Rosenblat I, Blushtein O. Impact of dispatcher assisted CPR on ROSC rates: A National Cohort Study. Am J Emerg Med. 2021;44:333-8. doi: 10.1016/j.ajem.2020.06.040.
- Leeb FA. Saving the savable: using bystanders to increase survival from out-of-hospital cardiac arrest (OHCA) in New York City. Doctoral Thesis, Monterey, California: Naval Postgraduate School; 2016. Available from: https://www.proquest.com/docview/1802506073.
- Kajino K, Iwami T, Daya M, Nishiuchi T, Hayashi Y, Ikeuchi H et al. Subsequent ventricular fibrillation and survival in out-of-hospital cardiac arrests presenting with PEA or asystole. Resuscitation. 2008;79(1):34-40.doi: 10.1016/j.resuscitation.2008.01.010.
- Wolbinski M, Swain AH, Harding SA, Larsen PD. Out-of-hospital Cardiac Arrest Patient Characteristics: Comparing ventricular arrhythmia and Pulseless Electrical Activity. Heart Lung Circ. 2016;25(7):639-44. doi:10.1016/j.hlc.2016.02.014.
- Meaney PA, Nadkarni VM, Kern KB, Indik JH, Halperin HR, Berg RA. Rhythms and outcomes of adult in-hospital cardiac arrest. Crit Care Med. 2010;38(1):101-8. doi: 10.1097/CCM.0b013e3181c12b07.
- Bergman R, Hiemstra B, Nieuwland W, Lipsic E, Absalom A, van der Naalt J et al. Long-term outcome of patients after out-of-hospital cardiac arrest in relation to treatment: a single-centre study. Eur Heart J Acute Cardiovasc Care. 2016;5(4):328-38. doi: 10.1177/2048872615618722.
- Peters GA, Ordoobadi AJ, Panchal AR, Cash RE. Differences in out- of-hospital cardiac arrest management and outcomes across urban, suburban, and rural settings. Prehosp Emerg Care. 2023;27(2):162-9. doi:10.1080/10903127.2022.2139074.
- Ringh M, Jonsson M, Nordberg P, Fredman D, Hasselqvist-Ax I, Håkansson F et al. Survival after Public Access Defibrillation in Stockholm, Sweden – A striking success. Resuscitation. 2015;91:1-7. doi: 10.1016/j.resuscitation.2014.12.009.
- Ro YS, Do Shin S, Song KJ, Hong SO, Kim YT, Lee DW et al. Public awareness and self-efficacy of cardiopulmonary resuscitation in communities and outcomes of out-of-hospital cardiac arrest: a multi-level analysis. Resuscitation. 2016;102:17-24. doi: 10.1016/j.resuscitation.2016.02.025.
- Hirlekar G. Cardiac arrest with emphasis on comorbidity and choice of treatment in acute coronary syndrome in the elderly. Doctoral Thesis, University of Gothenburg; 2020. Available from: https://gupea.ub.gu.se/handle/2077/67145.
- Lewandowski Ł, Mickiewicz A, Kędzierski K, Wróblewski P, Koral M, Kubielas G, et al. The Interaction Effect of Age, Initial Rhythm, and Location on Outcomes After Out-of-Hospital Cardiac Arrest: A Retrospective Cohort Study. J Clin Med. 2024;13:6426. doi: 10.3390/jcm13196426.
- Edin MG. Cardiopulmonary resuscitation in the frail elderly: clinical, ethical and halakhic issues. Isr Med Assoc J. 2007;9:177–9. Available from: https://www.ima.org.il/MedicineIMAJ/viewarticle.aspx?year=2007&vol=9&page=177.
- Gässler H, Helm M, Hossfeld B, Fischer M. Survival Following Lay Resuscitation. Dtsch Arztebl Int. 2020;117(51-52):871-877. doi: 10.3238/arztebl.2020.0871.
- Greif R, Bhanji F, Bigham BL, Bray J, Breckwoldt J, Cheng A, et al. Education, implementation, and teams: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2020;142(16_suppl_1):S222-83. doi: 10.1161/CIR.0000000000000915.
- Ravindra P, Shubha HS, Nagesh SK, Bhat R, Sahu AK, Chugh S et al. CPR challenge: Impact of a social media campaign on cardiopulmonary resuscitation awareness and skills among young adults − A quasi experimental study. Resuscitation Plus. 2024;19:100711. doi:10.1016/j.resplu.2024.100711.

Published under the Creative Commons Attribution 4.0 International License
