DELIRIUM ASSESSMENT AND MANAGEMENT IN EMERGENCY DEPARTMENT
Introduction
Delirium is an acute mental disorder, characterized by a disturbance of consciousness (qualitative), a fluctuating course and disorders of higher cognitive functions (disorders of orientation, memory, thinking and behavior). It develops over a short period of time (hours, days) and has a tendency for symptoms to vary throughout the day (1,2).
In the 11th revision of the ICD (International Classification of Diseases), delirium is defined as an etiologically non-specific organic cerebral syndrome that has the following characteristics:
- disturbance of consciousness and attention,
- global cognitive disorders (illusions, hallucinations, thought disorders, memory disorders, recall problems, disorientation…),
- psychomotor disorders,
- sleep and wakefulness rhythm disorders,
- emotional disorders (1,3,4).
Hyperactive delirium
Hyperactive delirium is a form of delirium, characterized by state of increased alertness and agitation. It is more often accompanied by hallucinations, delusions, agitation and inappropriate behavior of the patient (1,5).
Prominent psychomotor agitation is characteristic, patients are restless, excited, sometimes even aggressive towards themselves and their surroundings. Reactions to environmental stimuli such as light, touch or noise can be exaggerated. Various inappropriate behaviors occur, such as screaming, removing inserted medical equipment (peripheral and central channels, catheters, sutures…). Patients might have a tendency to flee. Hallucinations and illusions, disorientation and emotional lability are common. Patients act as if they have psychosis but without prodromes (3,5,6).
Hypoactive delirium
Hypoactive delirium is a subtype of delirium, characterized by reduced psychomotor activity, lethargy and reduced response to environmental stimuli, and apathy. This form is often overlooked, as we do not observe clear disturbing behavioral disorders in the patient (3,4).
Clinically, it manifests as psychomotor hypoactivity, patients are sleepy, may be unresponsive, have problems following their surroundings and focusing, are apathetic to their surroundings and interactions with other people. We can observe quantitative disorders of consciousness in the sense of somnolence and stupor, but patients may simply be less oriented in time, space and person. Problems with understanding, memory and judgment also stand out. It occurs more often as a result of somatic diseases. It is especially common in palliative care (3,7,8).
Mixed delirium
Mixed delirium is a combination of both hyperactive and hypoactive delirium. Patients have a combination of symptoms of the two types of delirium listed above, which alternate with each other (2,3).
Delirium due to alcohol withdrawal; delirium tremens
We speak of alcoholic delirium as an etiologically special form of delirium, as a severe complication of alcohol withdrawal syndrome. It manifests itself as a hyperactive form. It can occur during actual withdrawal from alcohol or during other conditions (infections, injuries,…) when the patient cannot consume alcohol due to the nature of the problems themselves. It manifests as agitation with confusion and disorientation; hallucinations and autonomic signs such as fever, hypertension, diaphoresis and tachycardia are common. Electrolyte disturbances can lead to rhythm disturbances, epileptic seizures or even sudden cardiac death. It usually lasts 3 to 4 days, but can take up to 10 days (5,9,10).
Delirium in elderly and frail patients
Elderly, frail patients are a high-risk population for the development of delirium, which is often associated with prolonged hospitalization and worse treatment outcomes. It is often difficult to recognize due to overlap with other pathologies of old age, such as dementia and depression. The symptoms are similar to those of other types, manifesting as attention deficit disorder, confusion, disorientation, disturbances of consciousness and behavior. The most common cause of delirium in elderly patients is infection, followed by hospitalization (change of environment) and worsening of underlying chronic diseases (11,12,13).
Delirium in oncologic patients and palliative care
In oncology and palliative care, delirium is a common and serious symptom. It mainly occurs in patients with advanced and end stages of the disease. It can be caused by an underlying disease, but often occurs as a result of treatment (chemotherapy, immunotherapy), associated pharmacotherapy (treatment with opioids), metabolic disorders, infections or dehydration. Treatment of delirium in palliative care focuses primarily on managing symptoms, alleviating suffering and improving patients’ quality of life. We use etiological treatment and treatment with medicinal and non-medicinal measures (3,14,15).
Epidemiology of delirium
Data on prevalence of delirium varies from study to study. Delirium should occur in about 10-15% of all hospitalized patients; it is much more common in those who are older than 65 years, some references report prevalence of more than 50% of this patient population. The occurrence is also related to hospitalizations, with higher incidence in surgical wards, where elderly patients are treated after injuries and fractures (even more than 50%), in intensive care units and in patients hospitalized for a malignant disease. Unrecognized delirium leads to longer hospitalization and higher mortality (3,16,17). According to some studies, delirium remains unrecognized in emergency departments (ED) in approximately 2/3 of cases (17,18).
Pathophysiology and etiology
The exact mechanisms that cause delirium are yet unknown, but it is most likely caused by reversible malfunction of the oxidative metabolism in the brain, responsible for changes in the metabolism of various substances, altered enzyme systems, and a more permeable blood-brain barrier or cell membranes. Disturbed metabolism of neurotransmitters and disturbances in the function of the right hemisphere, necessary for adequate attention, also play a role (3,19).
The pathophysiology of delirium is related to the action of various neurotransmitters; acetylcholine, dopamine, serotonin, gamma-aminobutyric (GABA) and glutamate. Acetylcholine plays an important role in memory, consciousness and attention. Dopamine is associated with disorders of attention, motivation and emotion regulation. Serotonin mainly affects mood (3,20).
Delirium also encompasses impairment of higher brain functions, centred in the cerebral cortex. Delirium development requires the involvement of several neurotransmitter systems, the cholinergic system being particularly important. This is the reason why drugs with anticholinergic properties very often cause delirium. By acting on muscarinic receptors, they affect subcortical cholinergic fibers and thus reduce the flow of neurotransmitters to the cortex and hippocampus. The mechanism of delirium that occurs during withdrawal from benzodiazepines and barbiturates is most likely related to hypersensitivity of GABA receptors. A similar mechanism is also present in delirium of alcoholic etiology (3,19,20).
A higher risk of delirium is present in the elderly and frail patient population. Risk factors that increase the likelihood of delirium are:
- age over 70 years,
- dementia (in many cases it is first diagnosed only later),
- male gender,
- poor eyesight and hearing,
- other associated cognitive disorders (mental retardation, psycho-organic changes),
- (chronic) abuse of alcohol and psychoactive substances,
- metabolic abnormalities (metabolic, electrolyte, elevated inflammatory parameters…) (3,5,19).
Causes of delirium are multiple. In very fragile patients, development of delirium can be precipitated by even a minor disturbance such as lack of sleep, urinary retention, dehydration and constipation. The most common causes are:
- side effects of drugs (psychotropic drugs such as antipsychotics, sedatives, antidepressants and anxiolytics, anticholinergics, opioid analgesics),
- withdrawal from drugs, polypharmacy,
- operative interventions (orthopedic and traumatological interventions in the elderly) and general anesthesia,
- hypoxia,
- pain,
- infections,
- acute diseases and exacerbations of chronic diseases,
- dehydration,
- immobility (3,5,21).
Causes of delirium can be easily remembered by mnemonic “I WATCH DEATH” shown in Table 1 (2,3,5).
Table 1: Causes of delirium (5)
| Mnemonic | Specific causes |
| I – nfectious | Sepsis, encephalitis, meningitis, syphilis |
| W – ithdrawal | Alcohol, barbiturates, sedatives, hypnotics |
| A – cute metabolic causes | Acidosis, electrolyte disturbances, liver and kidney failure, hypo/hyperglycemia, |
| T – rauma | Head injuries, burns |
| C – NS (cerebral nervous sistem) diseases | Cerebral hemorrhage/stroke, vasculitis, convulsions, tumors |
| H – ypoxia | Acute hypoxia, chronic lung diseases, hypotension, |
| D – eficiencies (vitamins, micronutrients) | vitamin B12, niacin, thiamine |
| E – nvironmental factors | Hypo/hyperthermia, endocrinopathies, diabetes, thyroid/adrenal gland diseases |
| A – cute vascular | Hypertensive crises, SAH, central venous sinus thrombosis |
| T – oxins/drugs/medications | Medicines, drugs, alcohol, pesticides, poisons, CO, cyanides |
| H – eavy metals | Lead, mercury |
SAH – subarachnoid hemorrhage; CO – carbon monoxide
Clinical signs and symptoms
Delirium can be heralded by prodromal signs such as restlessness, anxiety, fear, and hypersensitivity to light and sound (1).
The clinical picture develops in few hours to days. Manifestations of symptoms fluctuates over time, symptoms usually being more pronounced at night (2,3) (old clinical adage, “nights possess special powers”).
Patients may experience difficulties with orientation. Orientation in time is most often and first affected (difficulties in determining the part of the day are considered a sensitive indicator of delirium), spatial and personal orientation are less frequently affected (1).
Patients with delirium often have hallucinations; dreams and illusions can be intertwined. Perceptual disturbances are most often optical or auditory. Olfactory and tactile hallucinations occur less frequently. Hallucinations and experiences are often unpleasant, patients are often frightened, tense and anxious. Attention is also disturbed, the flow of thought is slowed down and incoherent (2,3).
Disorders of the autonomic nervous system may occur, such as skin erythema or pallor, sweat, tachycardia, arrhythmias, hypertension, vomiting, mydriasis and hyperthermia. These symptoms often occur in delirium that occurs as a result of withdrawal from alcohol, sedatives and hypnotics (1,2,3).
Memory disorders are present both in terms of difficulty with memorization and recall; patients can fill individual memory holes with confabulations. Patients are typically amnestic for the period of delirium. The rhythm of sleep and wakefulness is often completely reversed, but patients may have problems especially with insomnia (4,22).
The behavior of patients can be very extreme; on one hand, there can be psychomotor retardation, patients can be imperceptible and mutatic, and on the other hand, there can be very pronounced restlessness with loud and rapid speech. Patients can experience emotional disturbances, they can be very irritable and agitated, anxious, and emotionally numb. Depressed mood, confusion and thoughts of suspicion are often associated with delirium (2,3,23).
Diagnostic assesment
Diagnosis of delirium is clinical, suspicion for delirium is mostly based on history by family or caregivers and clinical exam. There are no specific diagnostic tests for delirium and even laboratory tests can only confirm a possible etiological cause of delirium (infection, metabolic disorders, electrolyte imbalance, etc.). To rule out somatic causes, CT and MR imaging can be performed, as also EEG recording of brain activity; these can demonstrate a bilateral, diffuse abnormality of the basic electrical activity with a slowing rate of the average frequency (1,2,3).
To make a diagnosis, we use the DSM-V (Diagnostic and Statistical Manual of Mental Disorders) criteria:
- disturbance in attention and consciousness,
- the disorder occurs quickly (a few hours to few days) and represents a change in patients condition, compared to their baseline behavior and clinical exam,
- disturbance in thinking (i.e. memory, disorientation, disturbances in speech, vision, perception),
- the disorder cannot be explained by another or previously existing neurological deficit,
- there is enough evidence in history, physical examination and laboratory tests that the disorder may be the result of illness, intoxication or withdrawal from a certain substance and a possible side effect) (2,24,25).
The bCAM and 4AT tests are used to help identify delirium, and the CAM-ICU scale is also used in intensive care units (25).
bCAM (Brief Confusion Assessment Method)
bCAM is a delirium screening tool and is a simplified version of the Confusion Assessment Method (CAM). It is adapted for settings where time for assessment limited (emergency centers, intensive care units). It focuses on 4 key features of delirium:
- acuteness of the onset of symptoms (anamnesis and/or hetero-anamnesis on the patient’s mental state and changes in the last 24 hours),
- attention disorders,
- disorganized thinking (we ask the patient simple questions such as “Does a stone float on water?” and evaluate the logic and appropriateness of the patient’s answers),
- altered level of consciousness (we assess whether the patient has signs of hypo- or hyperactive delirium – impaired consciousness, lethargy, restlessness, agitation).
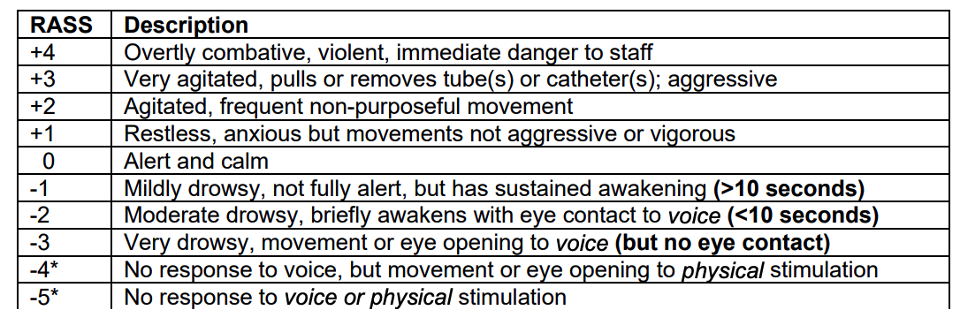
The Richmond-Agitation-Sedation-Scale (RASS) is also part of the assessment of delirium according to the bCAM scale. Figure 1 and Table 2 show a brief delirium screening tool; bCAM (26,27,28).
bCAM has proven to be a highly specific but less sensitive tool (27).
Figure 1: brief delirium screening (bCAM – brief Confusion Assessment Method). Adapted from (28).
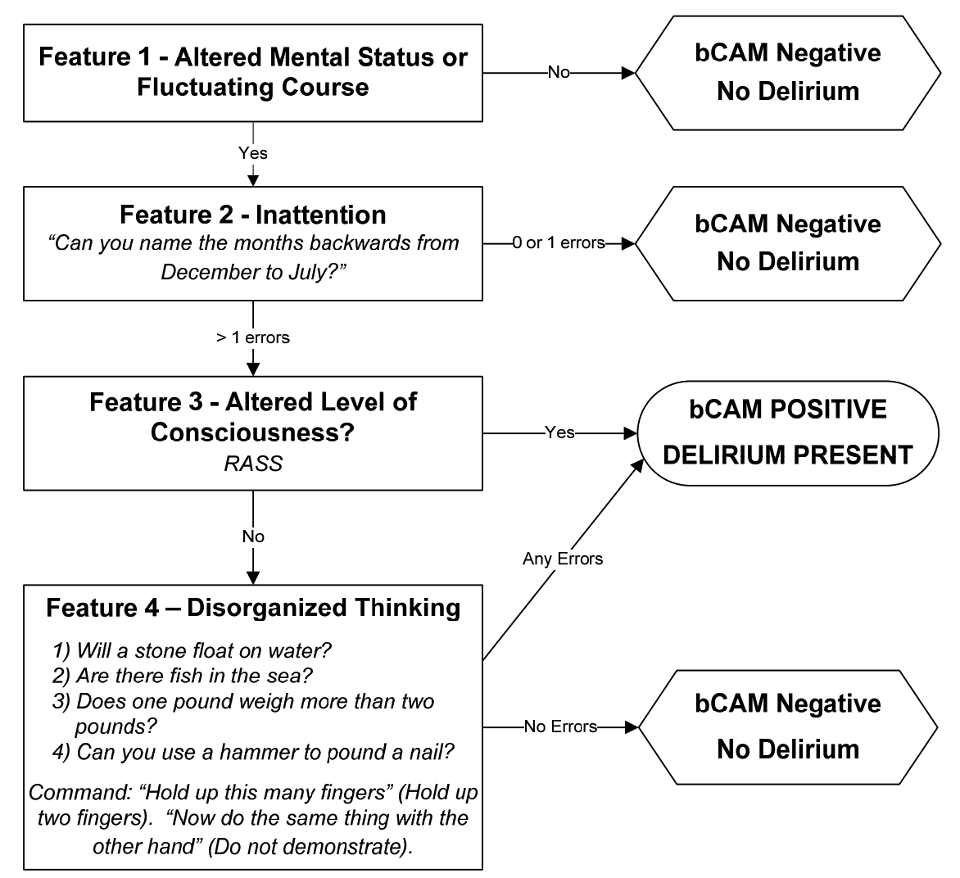
Table 2: RASSS (Richmond – Agitation – Sedation – Scale; Richmond Agitation and Sedation Scale). Adapted from (28).
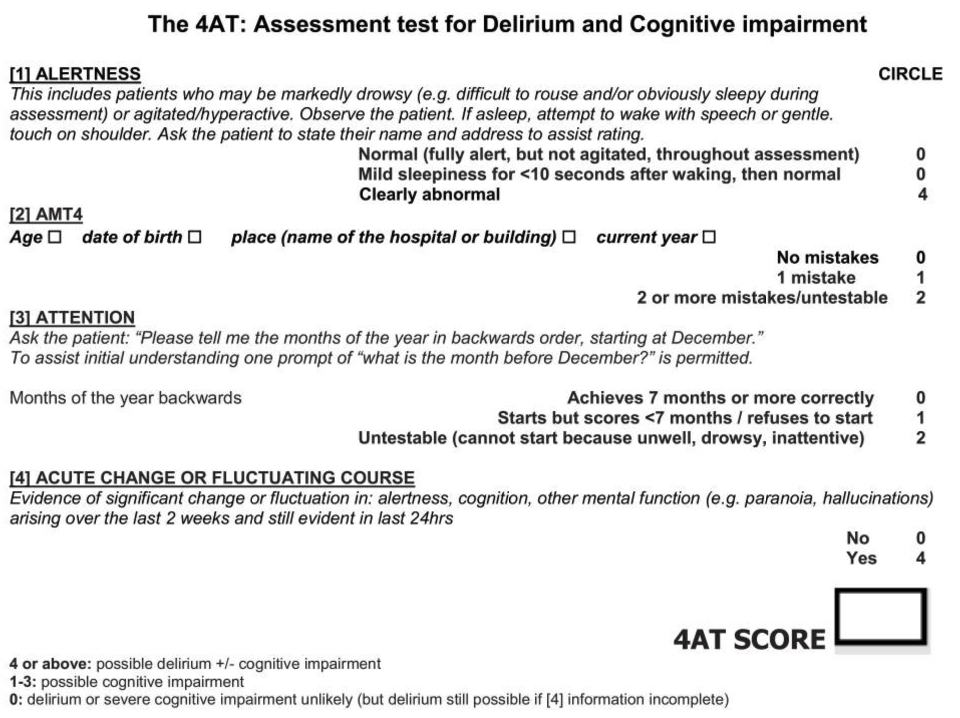
4A test
The 4A test is a simple and rapid screening test, suitable for use both in emergency departmets and other settings. We assess the patient’s alertness, acute onset and fluctuation of symptoms, attention and memory, and cognitive impairment. In research, the test has shown high diagnostic accuracy. Table 3 shows how 4AT test is performed (27,29,42).
Figure 2: 4 A test. Adapted from 42.
Differential diagnosis of delirium
Delirium is a condition characterized by acute and reversible disturbances of consciousness and cognition, and may also be accompanied by various neuropsychiatric symptoms. For appropriate managament and treatment, delirium must be recognized and distinguished from other similar conditions. We establish the diagnosis with a systematic auto or hetero-anamnesis (history), a detailed clinical examination, aided by laboratory and imaging tests. The most common differential diagnosis (alternative causes) are:
- dementia (both conditions are characterised by cognitive impairment; delirium, unlike dementia, occurs acutely and fluctuates in time. Dementia is chronic, progressive disease),
- depression (in both conditions, apathy and cognitive problems can be observed, in depression there should be no acute changes in consciousness),
- psychosis (hallucinations may occur in both cases, consciousness should not be disturbed in psychosis or any other “pure” psychiatric disease),
- stroke (both conditions can have a sudden onset with confusion; in stroke we generally observe focal neurological deficits, in delirium it is a diffuse impairment without clear lateralization),
- electrolyte and metabolic disorders (hypoglycemia, hypo/hypernatremia, hypoxia/hypercapnia), endocrinological conditions (hypo/hyperthyroidism, Addison’s crisis),
- sepsis,
- drug poisoning,
- intoxication with alcohol or other psychoactive substances,
- expansive lesions of the brain (tumors, hydrocephalus, hemorrhages, …) (3,18,31).
Delirium is an acute mental disorder, characterized by a qualitative disturbance of consciousness, a fluctuating course and disorders of higher cognitive functions such as disorders of orientation, memory, thinking and behavior.
Delirium management in emergency department
In emergency departments, doctors and other health-care providers often encounter delirium, so recognizing it is very important. We approach patient with possible delirium as any other patients in emergency medicine: primary (ABCDE) and secondary exam and in parallel obtain history from patients and caregivers, which is usually key to identifying changes in patient’s behavior. We supplement diagnostic assessment with laboratory and imaging tests, trying to identify the triggering factor of delirium. bCAM and 4AT tests can be used for screening and confirmation of diagnosis (31,32,33).
After establishment of a diagnosis, urgent causative etiologic treatment is the cornerstone of delirium management. Medications (antipsychotics and benzodiazepines) are used to control symptoms, not to treat the root causes of delirium (3).
Regarding elderly and fragile patients, we will also discuss plans for further treatment and safety, or appropriateness of hospitalization.
Treatment of delirium
Treatment of delirium is primarily etiological. By treating the underlying cause, symptoms of delirium may be reversed accordingly. In parallel, we must stabilize patients, provide them with cognitive support, and in most cases, also use supportive pharmacological treatment (3).
It is therefore of utmost importance to recognize delirium identify and treat its cause, to provide patients with an appropriate environment and support, and to use medication when necessary, while continuously monitoring the patient (34,35).
Non-pharmacologic treatment
It is necessary to provide patients with comfort, rest, and sufficient hydration and nutrition. Encouragement is needed in terms of location, time and personal orientation (clock, calendar, family photos, etc.). We should also encourage patients to use eyeglasses or hearing aids.
It is necessary to provide patients with a calm, familiar environment and to reduce noise. We should try to maintain a daily routine, paying special attention to sleep hygiene and rest. With physiotherapy and walking aids, we should try to mobilize patients as much as possible. Patients should also be provided with spiritual support as needed (33,36).
Pharmacologic treatment
The choice of medication depends on predominant symptom phenotype. Pharmacologic therapy with antipsychotics or benzodiazepines is not causal, but merely symptomatic. The pathophysiological mechanism of delirium hinges on imbalance between neurotransmitters, mostly with an excess of dopaminergic transmissions and a lack of cholinergic transmissions. Medication treatment is also based on this principle (3,37).
Haloperidol is an effective medication in most patients (except for withdrawal syndrome and poisoning with anticholinergics). We mainly use antipsychotics with predominantly hyperactive form, with symptoms of aggression, agitation and hallucinations:
- haloperidol (Haldol) – often used due to its fast-acting nature and favorable safety profile in short-term treatment,
- mild to moderate delirium: 0.5 – 3 mg intramuscularly or orally every 8 – 12 hours and every 1 hour if necessary. When a dose needs to be titrated, use 50% of the daily dose, which is divided into up to 3 daily doses,
- pronounced delirium with agitation: 1.5 – 3 mg intramuscularly or orally every 8 – 12 hours, up to a maximum daily dose of 30 mg,
- quetiapine (Kventiax, Seroquel)
- 12.5 – 50 mg per 12/24 hours up to a maximum daily dose of 200 mg,
- olanzapine (Zolrix, Zyprexa)
- 1.25 – 5 mg/24 hours orally or 2.5 – 5 mg/day intramuscularly up to a maximum daily dose of 20 mg,
- risperidone (Torendo, Rispolux)
- 0.25 – 2 mg orally, can be repeated every 2 hours up to a maximum daily dose of 6 mg.
Antipsychotics are prescribed in a lowest effective doses and are gradually discontinued when delirium subsides. Side effects manifest mainly due to their cholinergic effects, namely dry mouth, dizziness, headache, constipation, increased appetite and tachycardia (37,38).
For treatment of delirium tremens (severe alcohol withdrawal), clomethiazole (Hemineurin/Distraneurin) is most commonly used in Europe. It has hypnotic, sedative and anticonvulsant effects. Doses range between 200 – 400 mg, which can be repeated after one hour, and then every 2 – 3 hours, up to a maximum daily dose of 2 g. It is not recommended to use in intoxicated patients, as the drug can further suppress the central nervous system. When used for more than 10 days, addiction may develop, and side effects are mainly on the nervous system (respiratory center depression, drop in blood pressure). Some recent studies have also described the use of phenobarbital in patients with withdrawal symptoms, where better clinical outcomes were observed with the use of phenobarbital compared to monotherapy with benzodiazepines (37,39,40).
We also use benzodiazepines, with short half-life. They can be used in combination with antipsychotics for cases of severe hyperactive delirium. We most often use:
- oxazepam,
- 10 – 30 mg 3 – 4 times a day,
- midazolam (Dormicum),
- 2.5 – 5 mg orally or intravenously, up to a maximum of 15 mg in 24 hours,
- lorazepam (Loram)
- 0.5 – 1 mg 1x/day orally, 1 – 2 mg intramuscularly,
- diazepam
- 2 – 5 mg orally, 5 – 10 mg intravenously plus repeat if necessary.
According to some studies, delirium remains unrecognized in emergency departments in approximately 2/3 of cases. Unrecognized delirium leads to longer hospitalization and higher mortality.
Benzodiazepines play a role in the symptomatic treatment of delirium, especially in patients with hyperactive delirium, delirium in terminally ill oncology patients, and delirium during alcohol withdrawal. We must also be aware of side effects, which in the case of benzodiazepines are mainly confusion and agitation, and in case of overdose, respiratory depression, hypotension, nausea and vomiting may also occur (14,39,41).
In treatment of hypoactive delirium, benzodiazepines are avoided, the use of antipsychotics in low doses is recommended, atypicals are preferred (14,15,37).
Equally, prevention of delirium is critically important; this includes timely causal treatment of the disease, care for adequate hydration and nutrition, reduction of unnecessary hospitalizations and transports to emergency departments, reduced use of drugs that cause delirium and provision of a stimulating environment with social interactions (39).
In most patients, prognosis depends on cause of delirium; in general worse treatment outcomes are associated with older age, frailty, hypoactive delirium and longer duration of delirium. Literature reports hospital mortality of patients with delirium up to 18%, which is almost twice as high as in the population without delirium (3,4).
Summary
Delirium is a clinical syndrome of acute confusion and other cognitive disturbances, caused by a number of different factors and has a heterogeneous clinical picture. The main characteristic is a qualitative disturbance of consciousness, which in most cases is the result of other medical conditions. Delirium is generally divided into hypoactive, hyperactive and mixed types. Delirium is today highly prevalent in ED, especially in elderly, fragile and oncologic patients. Establishing a correct diagnosis can be challenging, and it is often overlooked, resulting in worse outcomes and increased mortality. Treatment is based on reversing the somatic cause, aided by symptom control with antipsychotics or benzodiazepines, and other non-pharmacologic and supportive measures.
References:
- Kogoj A. Delirij. Med Razgl. 1994;33:325-38.
- Pregelj P, Kores Plesničar B, Tomori M, Zalar B, Ziherl S. Psihiatrija. Ljubljana: Psihiatrična klinika; 2013.
- Wilson JE, Mart MF, Cunningham C, Shehabi Y, Girard TD, MacLullich AMJ, Slooter AJC, Ely EW. Delirium. Nat Rev Dis Primers. 2020 Nov 12;6(1):90. doi: 10.1038/s41572-020-00223-4. Erratum in: Nat Rev Dis Primers. 2020 Dec 1;6(1):94. doi: 10.1038/s41572-020-00236-z.
- Ramírez EML, Schoo C, Paul M. Delirium. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470399/ [Accessed 2 Deceber 2024].
- Harrison P, Cowen P, Burns T, Fazel M. Shorter Oxford Textbook of Psychiatry. OUP; 2018.
- Springer B. Hyperactive Delirium with Severe Agitation. Emerg Med Clin North Am. 2024; 42(1):41-52.
- Rosen JH, Bieber E, Matta SE, Sayde GE, Fedotova NO, deVries J, Rafferty M, Stern TA. Hypoactive Delirium: Differential Diagnosis, Evaluation, and Treatment. Prim Care Companion CNS Disord. 2024 Feb 8;26(1):23f03602. doi: 10.4088/PCC.23f03602..
- van Velthuijsen EL, Zwakhalen SMG, Mulder WJ, Verhey FRJ, Kempen GIJM. Detection and management of hyperactive and hypoactive delirium in older patients during hospitalization: a retrospective cohort study evaluating daily practice. Int J Geriatr Psychiatry. 2018 Nov;33(11):1521-1529. doi: 10.1002/gps.4690. Epub 2017 Feb 14.
- Kaye AD, Staser AN, Mccollins TS, Zheng J, Berry FA, Burroughs CR. Delirium Tremens: A Review of Clinical Studies. Cureus. 2024 Apr 4;16(4):e57601. doi: 10.7759/cureus.57601.
- Grover S, Ghosh A. Delirium Tremens: Assessment and Management. J Clin Exp Hepatol. 2018 Dec;8(4):460-470. doi: 10.1016/j.jceh.2018.04.012
- Fong TG, Inouye SK. The inter-relationship between delirium and dementia: the importance of delirium prevention. Nat Rev Neurol. 2022 Oct;18(10):579-596. doi: 10.1038/s41582-022-00698-7.
- Bellelli G, Brathwaite JS, Mazzola P. Delirium: A Marker of Vulnerability in Older People. Front Aging Neurosci. 2021 Apr 30;13:626127. doi: 10.3389/fnagi.2021.626127. PMID: 33994990; PMCID: PMC8119654.
- Han QYC, Rodrigues NG, Klainin-Yobas P, Haugan G, Wu XV. Prevalence, Risk Factors, and Impact of Delirium on Hospitalized Older Adults With Dementia: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc. 2022 Jan;23(1):23-32.e27. doi: 10.1016/j.jamda.2021.09.008.
- Ebert Moltara M, Bernot M (ur.). 2023. Paliativna oskrba odraslih bolnikov z rakom v Sloveniji. Onkološki inštitut Ljubljana.
- Grassi L, Caraceni A, Mitchell AJ, Nanni MG, Berardi MA, Caruso R, Riba M. Management of delirium in palliative care: a review. Curr Psychiatry Rep. 2015 Mar;17(3):550. doi: 10.1007/s11920-015-0550-8.
- Émond M, Boucher V, Carmichael PH, Voyer P, Pelletier M, Gouin É, et al. Incidence of delirium in the Canadian emergency department and its consequences on hospital length of stay: a prospective observational multicentre cohort study. BMJ Open. 2018 Mar 8;8(3):e018190. doi: 10.1136/bmjopen-2017-018190.
- Boucher V, Lamontagne ME, Nadeau A, Carmichael PH, Yadav K, Voyer P, Pelletier M, Gouin É, Daoust R, Berthelot S, Morin M, Lemire S, Minh Vu TT, Lee J, Émond M. Unrecognized Incident Delirium in Older Emergency Department Patients. J Emerg Med. 2019 Oct;57(4):535-542. doi: 10.1016/j.jemermed.2019.05.024.
- Tintinalli J, Stapczynski S, John Ma O, et al. Tintinalli’s Emergency medicine 8th ed. New York: McGrawHill Eduacation; 2016.
- Maclullich AM, Ferguson KJ, Miller T, de Rooij SE, Cunningham C. Unravelling the pathophysiology of delirium: a focus on the role of aberrant stress responses. J Psychosom Res. 2008 Sep;65(3):229-38. doi: 10.1016/j.jpsychores.2008.05.019. PMID: 18707945; PMCID: PMC4311661.
- McKay TB, Khawaja ZQ, Freedman IG, Turco I, Wiredu K, Colecchi T, Akeju O. Exploring the Pathophysiology of Delirium: An Overview of Biomarker Studies, Animal Models, and Tissue-Engineered Models. Anesth Analg. 2023 Dec 1;137(6):1186-1197. doi: 10.1213/ANE.0000000000006715.
- Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014 Mar 8;383(9920):911-22. doi: 10.1016/S0140-6736(13)60688-1. Epub 2013 Aug 28. PMID: 23992774; PMCID: PMC4120864.
- Stollings JL, Kotfis K, Chanques G, Pun BT, Pandharipande PP, Ely EW. Delirium in critical illness: clinical manifestations, outcomes, and management. Intensive Care Med. 2021 Oct;47(10):1089-1103. doi: 10.1007/s00134-021-06503-1.
- Martins S, Fernandes L. Delirium in elderly people: a review. Front Neurol. 2012 Jun 19;3:101. doi: 10.3389/fneur.2012.00101.
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association.
- Alexander SK, Needham E. Diagnosis of delirium: a practical approach. Pract Neurol. 2023 Jun;23(3):192-199. doi: 10.1136/pn-2022-003373.
- Han JH, Wilson A, Vasilevskis EE, Shintani A, Schnelle JF, Dittus RS, et al. Diagnosing delirium in older emergency department patients: validity and reliability of the delirium triage screen and the brief confusion assessment method. Ann Emerg Med. 2013 Nov;62(5):457-465. doi: 10.1016/j.annemergmed.2013.05.003. Epub 2013 Jul 31. PMID: 23916018; PMCID: PMC3936572.
- Mariz J, Costa Castanho T, Teixeira J, Sousa N, Correia Santos N. Delirium Diagnostic and Screening Instruments in the Emergency Department: An Up-to-Date Systematic Review. Geriatrics (Basel). 2016 Sep 1;1(3):22. doi: 10.3390/geriatrics1030022.
- Han JH. Brief Confusion Assessment Method (bCAM) Instruction Manual. Version 1.0. Nashville, TN: Vanderbilt University School of Medicine; 2015. Available from: https://eddelirium.org/wp-content/uploads/2016/05/bCAM-Training-Manual-Version-1.0-10-15-2015.pdf
- MacLullich AM, Shenkin SD, Goodacre S, Godfrey M, Hanley J, Stíobhairt A, Lavender E, Boyd J, Stephen J, Weir C, MacRaild A, Steven J, Black P, Diernberger K, Hall P, Tieges Z, Fox C, Anand A, Young J, Siddiqi N, Gray A. The 4 ‘A’s test for detecting delirium in acute medical patients: a diagnostic accuracy study. Health Technol Assess. 2019 Aug;23(40):1-194. doi: 10.3310/hta23400.
- Tieges Z, Maclullich AMJ, Anand A, Brookes C, Cassarino M, O’connor M, et al. Diagnostic accuracy of the 4AT for delirium detection in older adults: systematic review and meta-analysis. Age Ageing. 2021 May 5;50(3):733-743. doi: 10.1093/ageing/afaa224. PMID: 33951145; PMCID: PMC8099016.
- LaMantia MA, Messina FC, Hobgood CD, Miller DK. Screening for delirium in the emergency department: a systematic review. Ann Emerg Med. 2014 May;63(5):551-560.e2. doi: 10.1016/j.annemergmed.2013.11.010..
- Saviano A, Zanza C, Longhitano Y, Ojetti V, Franceschi F, Bellou A, Voza A, Ceresa IF, Savioli G. Current Trends for Delirium Screening within the Emergency Department. Medicina (Kaunas). 2023 Sep 8;59(9):1634. doi: 10.3390/medicina59091634. PMID: 37763753;
- Lee S, Gottlieb M, Mulhausen P, Wilbur J, Reisinger HS, Han JH, Carnahan R. Recognition, prevention, and treatment of delirium in emergency department: An evidence-based narrative review. Am J Emerg Med. 2020 Feb;38(2):349-357. doi: 10.1016/j.ajem.2019.158454.
- Jagodič HK, Jagodič K, Pregelj P. Obravnava bolnika z delirijem. Zdrav Vestn. 2009;78:473-80.
- Grover S, Avasthi A. Clinical Practice Guidelines for Management of Delirium in Elderly. Indian J Psychiatry. 2018 Feb;60(Suppl 3):S329-S340. doi: 10.4103/0019-5545.224473.
- Faeder M, Hale E, Hedayati D, Israel A, Moschenross D, Peterson M et al. Preventing and treating delirium in clinical settings for older adults. Ther Adv Psychopharmacol. 2023 Sep 8;13:20451253231198462. doi: 10.1177/20451253231198462.
- Sadlonova M, Duque L, Smith D, Madva EN, Amonoo HL, Vogelsang J, Staton SC, von Arnim CAF, Huffman JC, Celano CM. Pharmacologic treatment of delirium symptoms: A systematic review. Gen Hosp Psychiatry. 2022 Nov-Dec;79:60-75. doi: 10.1016/j.genhosppsych.2022.10.010.
- Burry L, Mehta S, Perreault MM, Luxenberg JS, Siddiqi N, Hutton B et al. Antipsychotics for treatment of delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev. 2018 Jun 18;6(6):CD005594. doi: 10.1002/14651858.CD005594.pub3.
- Grover S, Ghosh A. Delirium Tremens: Assessment and Management. J Clin Exp Hepatol. 2018 Dec;8(4):460-470. doi: 10.1016/j.jceh.2018.04.012.
- Punia K, Scott W, Manuja K, Campbell K, Balodis IM, MacKillop J. SAEM GRACE: Phenobarbital for alcohol withdrawal management in the emergency department: A systematic review of direct evidence. Acad Emerg Med. 2024 May;31(5):481-492. doi: 10.1111/acem.14788.
- Hui D. Benzodiazepines for agitation in patients with delirium: selecting the right patient, right time, and right indication. Curr Opin Support Palliat Care. 2018 Dec;12(4):489-494. doi: 10.1097/SPC.0000000000000395.
- Hui D. Benzodiazepines for agitation in patients with delirium: selecting the right patient, right time, and right indication. Curr Opin Support Palliat Care. 2018 Dec;12(4):489-494. doi: 10.1097/SPC.0000000000000395.

Published under the Creative Commons Attribution 4.0 International License
