APPLICATION OF NONINVASIVE VENTILATION IN EMERGENCY MEDICINE: CURRENT STRATEGIES AND CHALLENGES
Introduction
Acute respiratory failure (ARF) is one of the most urgent and demanding situations in emergency medicine and often requires rapid and effective therapy to avoid further complications and mortality (1). Traditional methods of invasive ventilation, such as endotracheal intubation and mechanical ventilation, are associated with an increased risk of complications, such as infections, barotrauma, and prolonged hospitalization (2). Non-invasive ventilation strategies have recently become increasingly important because of their effectiveness in avoiding these complications and improving patient outcomes. Noninvasive ventilation (NIV), including high-flow nasal cannula (HFNC), continuous positive airway pressure (CPAP), and bilevel positive airway pressure (BiPAP), is increasingly used in emergency settings to manage patients with acute respiratory failure. However, they are also not without risks (3). The approach to treating ARF is stepwise and includes a gradual increase in support from a nasal catheter, through HFNC and NIV, to invasive mechanical ventilation (IMV), a device for extracorporeal CO2 removal (ECCO2R), and a device for extracorporeal membrane oxygenation (ECMO) (Fig 1) (1). Some patients may need to be transferred to intensive care units for escalated respiratory support after the initial respiratory support is initiated in emergency medicine departments. However, some patients can be thoroughly cared for in emergency medicine departments if the problem is identified in time and if they are adequately cared for using the correct respiratory support modality (4).
This study aims to analyze the existing strategies for applying NIV in emergency medicine, investigate the advantages and limitations of these methods, and discuss their applications in different emergency scenarios. In addition, the benefits of non-invasive versus invasive methods were compared, including improved mortality and reduced need for intubation.
Potential applications of noninvasive ventilation in emergency medicine
In emergency medicine, rapid intervention and appropriate airway management are essential for the successful management of patients with acute respiratory failure. ARF can be caused by various conditions, including acute exacerbation of chronic obstructive pulmonary disease (COPD), cardiogenic pulmonary edema, hypoxemic respiratory failure, and infectious diseases such as pneumonia or sepsis (4,5).
Traditionally, invasive ventilation has been the first-line therapy for these patients; however, because of the risks associated with endotracheal intubation, noninvasive methods are increasingly preferred. The main advantages of NIV in emergencies include reducing the need for endotracheal intubation, reducing the risk of nosocomial infections, improving patient comfort, facilitating breathing without sedation, and accelerating recovery time (4).
In emergency settings, noninvasive methods are often used in patients with cardiogenic pulmonary edema or COPD because they allow rapid stabilization without requiring intubation, which is more effective in specific patient groups (6,7).
Strategies for the management of acute respiratory failure
The most commonly used noninvasive strategies for patients with acute respiratory failure include CPAP, BiPAP, and HFNC. These methods provide respiratory support, improve the ventilation-perfusion ratio, and reduce the workload on the lungs and heart.
Non-invasive ventilation (NIV), including HFNC, CPAP, and BiPAP, is increasingly favored in managing acute respiratory failure due to its ability to reduce the need for intubation, lower infection risks, and improve patient outcomes in emergency settings.
Continuous positive airway pressure (CPAP)
CPAP provides a constant positive airway pressure, prevents alveolar collapse, and allows better oxygenation. This method is beneficial for patients with cardiogenic pulmonary edema and acute exacerbations of COPD. Studies have shown that CPAP reduces the need for intubation and reduces mortality in patients with acute respiratory failure in emergency settings (8).
Bilevel-positive airway pressure (BiPAP)
BiPAP induces pressure changes during inspiration and expiration, further facilitating breathing in patients with hypercapnia, such as those with COPD. In emergency settings, BiPAP is often used as first-line therapy for patients with exacerbations of chronic lung diseases (9).
High-flow nasal cannula (HFNC)
HFNC is a relatively new technology that delivers warm and humidified oxygen at high flow rates through the nasal cannula. Studies have shown that HFNC may be an effective alternative for patients with hypoxemic respiratory failure, especially when standard oxygen therapy is insufficient. HFNC also has an advantage over CPAP and BiPAP in terms of greater patient comfort and a reduced risk of side effects (10).
Noninvasive Negative Pressure Ventilation (NPV)
Negative ventilation involves the creation of negative pressure around the chest and abdomen to allow lung expansion during inspiration, as opposed to positive ventilation, in which air is actively forced into the lungs by positive pressure. Historically, NPV was popular in treating poliomyelitis with devices such as the “iron lung,” but its use in acute and chronic respiratory failure has been re-examined.
Recent research has shown that NPV can be used in patients with hypercapnic respiratory failure, especially in combination with a high-flow nasal cannula (HFNC). This combination improves respiratory function without the need for invasive ventilation. For example, Imitazione et al. (2021) described a patient with acute respiratory failure and muscular dystrophy in whom they combined NPV and HFNC and noted significant improvements in respiratory parameters without the need for invasive ventilation (11).
Additionally, NPV has gained renewed attention during the COVID-19 pandemic, when combinations of various non-invasive methods, including NPV, have been shown to reduce hypoxia and improve respiratory mechanics. Chandrasekaran and Monikandan (2022) highlighted the importance of NPV in combination with an oxygen mask during the treatment of COVID-19 patients, leading to positive clinical outcomes (12). Although NPV is not as widely used as other methods, research suggests the potential utility of this method in emergency medicine, particularly in patients with chronic lung disease and severe respiratory failure.
Noninvasive ventilation in emergency medicine
In emergency medical settings, the rapid use of non-invasive ventilation can significantly improve outcomes in patients with acute respiratory failure. Non-invasive ventilation methods, such as CPAP and BiPAP, can be used in prehospital settings, allowing for earlier stabilization of patients. In hospital settings, using NIV in emergency departments has reduced mortality, the need for intubation, and intensive care unit stays (11). Given these general advantages, NIV specific applications in conditions such as cardiogenic pulmonary edema and COPD exacerbations demonstrate its critical role in emergency medicine.
While non-invasive ventilation offers significant benefits, its use in emergency medicine is challenging due to the need for rapid decision-making and proper staff training. Timely identification of patients who will benefit from NIV and exploring combination therapies, such as HFNC with BiPAP, remain critical areas for improving outcomes.
Use of NIV in acute COPD exacerbations
COPD is one of the most common causes of respiratory failure in the emergency setting. NIV, especially BiPAP, is key to managing these patients, as it helps reduce hypercapnia and facilitates breathing. According to a meta-analysis by Sakuraya et al. (2021), the use of NIV reduced the risk of intubation in patients with COPD by 75% (7).
Cardiogenic pulmonary edema
CPAP is particularly beneficial in patients with cardiogenic pulmonary edema because it helps to reduce cardiac preload and afterload, thereby improving cardiac function and facilitating breathing. This method can significantly reduce the risk of invasive ventilation in patients with acute heart failure (13).
Hypoxemic respiratory failure
HFNC is increasingly used in patients with hypoxemic respiratory failure, especially in those who are not candidates for intubation. HFNC allows for better oxygenation with greater patient comfort, a key advantage in emergencies (12). In comparison, our study showed that the use of high levels of positive end-expiratory pressure (PEEP) via noninvasive ventilation (NIV) is safe and effective in patients with COVID-19-associated acute respiratory distress syndrome (ARDS) (14). The effectiveness of this method is evident in the early stages of treatment, where the use of NIV avoids intubation in most patients, with a reduction in mortality among patients who remain on NIV (8).
Monitoring of the application of non-invasive mechanical ventilation
It is vital to closely monitor patients’ vital and respiratory parameters during non-invasive mechanical ventilation. This can be a challenge for the busy bustle of the emergency department. Timely recognition of inadequate respiratory support (NIV failure) prevents postponement of imminent intubation, which is associated with worse clinical outcomes (15). Many scores have been obtained for this purpose. One such score is HACOR, which has proven to be an excellent predictive tool for NIV failure (2,14,16).
Discussion
Although non-invasive ventilation has significant advantages, its implementation in emergency medicine is challenging. The need for rapid patient evaluation and decision-making regarding an appropriate ventilation strategy can be challenging, particularly in patients with mixed forms of respiratory failure.
One of the key challenges is the timely identification of patients who will benefit from noninvasive ventilation without missing the point when invasive ventilation is required. In addition, adequate training of the medical staff in the proper use and monitoring of patients on NIV is necessary, as improper use can lead to deterioration of the condition and the need for invasive ventilation.
Studies have shown that combining different noninvasive methods, such as HFNC and BiPAP, is effective in certain patients, especially during the COVID-19 pandemic when respiratory symptoms and failure are more pronounced (2). More research is needed to better understand the effects of combination therapies and their long-term effectiveness in emergency settings.
Conclusion
Noninvasive ventilation is a key emergency medicine method for treating patients with acute respiratory failure. Its advantages include a reduced risk of invasive complications and improved patient comfort, making it the preferred approach in many emergencies. However, careful evaluation of patients and appropriate training of the medical staff are required to maximize the benefits of this method. With further research and technological improvements, noninvasive ventilation methods will play an increasingly important role in emergency medicine.
References
- Satici C, López-Padilla D, Schreiber A, Kharat A, Swingwood E, Pisani L et al. ERS International Congress, Madrid, 2019: highlights from the Respiratory Intensive Care Assembly. ERJ Open Res. 2020 Mar 9;6(1):00331-2019. doi: 10.1183/23120541.00331-2019.
- Karković N, Šitum I, Lovrić D, Erceg A, Mamić G, Džaja N, et al. Učinkovitost i komplikacije neinvazivne respiratorne potpore, posebice liječenja s kontinuiranim pozitivnim tlakom u dišnim putevima kod COVID bolesnika. Medicina Fluminensis: Medicina Fluminensis, 60 (1), 28-35. https://doi.org/10.21860/medflum2024_313682
- Gay PC. Complications of noninvasive ventilation in acute care. Respir Care. 2009 Feb;54(2):246-57; discussion 257-8.
- Scquizzato T, Imbriaco G, Moro F, Losiggio R, Cabrini L, Consolo F et al. Non-Invasive Ventilation in the Prehospital Emergency Setting: A Systematic Review and Meta-Analysis. Prehosp Emerg Care. 2023;27(5):566-574. doi: 10.1080/10903127.2022.2086331.
- Rose L, Gerdtz MF. Review of non-invasive ventilation in the emergency department: clinical considerations and management priorities. J Clin Nurs. 2009 Dec;18(23):3216-24. doi: 10.1111/j.1365-2702.2008.02766.x.
- Schmitt FCF, Gruneberg D, Schneider NRE, Fögeling JO, Leucht M et al. Non-Invasive Ventilation as a Therapy Option for Acute Exacerbations of Chronic Obstructive Pulmonary Disease and Acute Cardiopulmonary Oedema in Emergency Medical Services. J Clin Med. 2022 Apr 29;11(9):2504. doi: 10.3390/jcm11092504.
- Sakuraya M, Okano H, Masuyama T, Kimata S, Hokari S. Efficacy of non-invasive and invasive respiratory management strategies in adult patients with acute hypoxaemic respiratory failure: a systematic review and network meta-analysis. Crit Care. 2021 Nov 29;25(1):414. doi: 10.1186/s13054-021-03835-8.
- Šitum I, Hrvoić L, Erceg A, Mandarić A, Karmelić D, Mamić G et al. D. CPAP vs HFNC in treatment of patients with COVID-19 ARDS: A retrospective propensity-matched study. Can J Respir Ther. 2024 Oct 31;60:164-172. doi: 10.29390/001c.125145.
- Khilnani GC, Banga A. Noninvasive ventilation in patients with chronic obstructive airway disease. Int J Chron Obstruct Pulmon Dis. 2008;3(3):351-7. doi: 10.2147/copd.s946.
- Abe T, Takagi T, Fujii T. Update on the management of acute respiratory failure using non-invasive ventilation and pulse oximetry. Crit Care. 2023 Mar 21;27(1):92. doi: 10.1186/s13054-023-04370-4.
- Imitazione P, Annunziata A, Lanza M, Fiorentino G. Combined high flow nasal cannula and negative pressure ventilation as a novel respiratory approach in a patient with acute respiratory failure and limb-girdle muscular dystrophy. Acta Myol. 2021 Jun 30;40(2):101-104. doi: 10.36185/2532-1900-049.
- Chandrasekaran K, Monikandan Shaji A. “The role of a negative pressure ventilator coupled with oxygen helmet against COVID-19: a review.” Research on Biomedical Engineering [Internet]. 2022 Mar 1 [cited 2024 Dec 11];38(1):267–78. Available from: https://link.springer.com/article/10.1007/s42600-021-00149-0
- Mina B, Newton A, Hadda V. Noninvasive Ventilation in Treatment of Respiratory Failure-Related COVID-19 Infection: Review of the Literature. Can Respir J. 2022 Aug 31;2022:9914081. doi: 10.1155/2022/9914081.
- Šitum I, Hrvoić L, Mamić G, Džaja N, Popović Z, Karković N et al. Efficacy and Safety of High PEEP NIV in COVID-19 Patients. Disaster Med Public Health Prep. 2024 May 30;18:e97. doi: 10.1017/dmp.2024.85.
- Liengswangwong W, Yuksen C, Thepkong T, Nakasint P, Jenpanitpong C. Early detection of non-invasive ventilation failure among acute respiratory failure patients in the emergency department. BMC Emerg Med. 2020 Oct 7;20(1):80. doi: 10.1186/s12873-020-00376-1.
- Duan J, Han X, Bai L, Zhou L, Huang S. Assessment of heart rate, acidosis, consciousness, oxygenation, and respiratory rate to predict noninvasive ventilation failure in hypoxemic patients. Intensive Care Med. 2017 Feb;43(2):192-199. doi: 10.1007/s00134-016-4601-3.
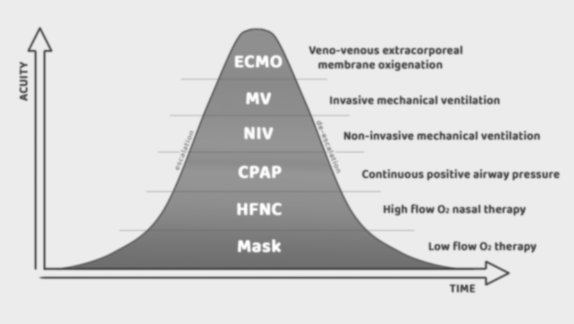
Figure 1. Stepwise approach to treating acute respiratory failure

Published under the Creative Commons Attribution 4.0 International License
